A 60 yr old female with polyarthritis and bilateral pedal edema
Hello everyone! I’m Rohini , an intern posted in General medicine department.
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio.
Here is a case i have seen:
A 60 yr old women presented to causality with
Complaints of Bilateral knee pain(aggravated) since
5days
Bilateral pedal edema since 5 days
She worked as a farmer for 35 years but from past 10 years she stopped going to work due to pain in both knee joints.
Patient was apparently alright 10 years back then she had h/o fever which lasted for about 3 to 4 days and subsided on taking paracetamol prescribed by local doctor. After that she felt pain in bilateral ankle joints which is associated with swelling for which she used medications ( no proper record about medication) which gave her symptomatic relief.
Then after 2 months , gradually it started involving her knees, shoulders, elbow, wrist . The pattern of involvement couldn’t be properly explained by the patient.and she even noticed deformity ( hallux varus type) of her right great toe.
Patient complained of Early morning stiffness which lasts for about 1 hour and gets relieved with work.
She was using on and off pain medications since 10 years
Patient went to multiple hospitals and used different medications (no proper records)
Patient complained of back pain 5 years ago and used Lumbar sacral belt for 2 months ( prescribed by local doctor).it got subsided completely .
One year back , she used to walk normally.and then she underwent Right Total knee replacement surgery and left TKR surgery was delayed due to covid pandemic.After 2months she started walking with help of stick. Since then she is walking with stick. And from 15days she is not able to walk due to pain.
She came to our hospital with complaints of Bilateral knee pain which was aggravated since 5 days which is associated with swelling in the both lower limbs.and Bilateral pedal oedema since 5 days (Pitting type up to knee)
Not a know case of DM,HTN,Thyroid disorder, TB
Patient developed bilateral lower limb cellulites 5 days back and also pressure necrotic patch on lower 1/3 rd posterior aspect of left leg for Which general surgery referral was taken.
Left lower limb arterial and venous doppler was done which showed:
Orthopaedic referral was taken in view of left knee swelling and pain.
X-ray of left knee:
Usg of left knee joint:
And adviced synovial fluid aspiration -
As synovial fluid aspirated was minimal . It was not sufficient enough for microbiological study.
•General examination :
Patient is conscious,coherent and cooperative. Oriented to time and place. Heavily built.
Pallor- present (mild)
Icterus- Absent
No cyanosis,clubbing, lymphadenopathy
Vitals: temp- afebrile
BP- 130/70 mmhg
PR-96bpm
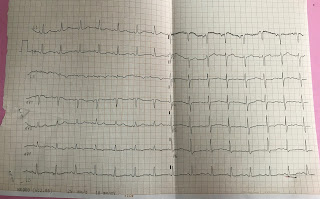
• CVS Examination:
Inspection-
Shape of chest-bilaterally symmetrical
Trachea-central in position
Jvp -raised
Apical impulse couldn't be seen.
Precordial and epigastric pulsations *absent
No visible scars,sinuses,engorged veins*
Palpation-
Apexbeat- couldn't be appreciated as pt is obese .
Parasternal heave,grade1 ,over left parasternal line
No palpable thrill ,no tenderness
Auscultation-
S1,s2 heard in pulmonary,mitral,tricuspid areas
Nomurmurs
•Respiratory Examination:
Normal vesicular breath sounds,
Bilateral air entry present
Trachea - central
Wheeze - absent
Crepts + bilaterally in isa ,iaa,inter scapular and mammary areas
Per Abdomen: soft , non tender
CNS : No FAD
• joint Examination:
Tenderness Restriction of movement
Lt Rt Lt Rt
TMJ - - - -
Shoulder:- - - -
Elbow - - - -
Wrist + + + +
MCP - - - -
IPJ
Distal - - - -
Proximal - - + +
Hip - - - -
Knee + + + +
Ankle + + + +
MTP + + + -
Intertarsal. + + + +
• EULAR criteria :
Joint distribution:
> 10 joints ( atleast one small joint) : score of 5
Serology: RA factor negative: 0
Symptoms duration:
> 6 weeks: score of 1
Acute phase reactants:score of 1
Crp negative
Esr raised
Total: 7
• Investigations:
Outside hospital reports:
Total counts : 21,500 29,500 28,700 32,600
Sr.Creatinine: 3 3.5 3 2.9
Blood Urea : 56 86 119 58
Total bilirubin : 5.2 6.1 6.6 7.7
Direct bilirubin: 2.6 3.1 4.5 4
ALP : 463 239 182 190
In our hospital:
•On the day of admission:









































Comments
Post a Comment